肝腸鈣粘蛋白CDH17:單抗、雙抗、CAR T“多管齊下”,胃腸道癌GIC重磅靶點!
日期:2023-03-27 14:58:09
近年來,胃腸道癌(Gastrointestinal carcinoma, GIC)的靶向治療逐漸成為研究的熱點,越來越多的靶點被發現,如EGFR、HER-2、PD-1、CTLA-4、VEGF、DDR1、LAG-3、MUC1、TIGIT、CLDN18.2等。新型靶向治療藥物還在不斷涌現,美國制藥巨頭勃林格殷格翰Boehringer Ingelheim近期開發了一款創新型基于CDH17的雙特異性抗體CDH17/TRAILR2/(BI 905711),已處于I/II期臨床階段,用于胃癌、胰腺癌、食管癌、膽管癌等胃腸道癌。BI 905711可同時結合腫瘤細胞表面的CDH17和死亡受體TRAILR2,誘導腫瘤細胞凋亡,對表達CDH17的正常細胞無損傷。
此外,香港生物制藥公司Arbele的CDH17單抗(ARB102)和雙特異性抗體CDH17/CD3(ARB202),正處于臨床前研究階段,用于治療胰腺癌、膽管癌等實體瘤。另有研究報道,一款針對CDH17的VHH1-CAR T細胞治療,可特異性根除表達CDH17的神經內分泌腫瘤NET、胃癌、胰腺癌以及結直腸癌細胞。因此,CDH17作為鈣黏蛋白超家族的新成員,成為開發更安全的實體瘤免疫療法的重磅靶點,尤其是胃腸道癌!
1. 什么是鈣黏蛋白超家族?
鈣黏蛋白(Cadherins)是一類介導鈣依賴型細胞間黏附的粘附分子超家族。家族成員眾多,根據結構不同可分為經典鈣黏蛋白(如E-鈣黏蛋白和N-鈣黏蛋白)、橋粒鈣黏蛋白、原鈣黏蛋白、七次跨膜鈣黏蛋白和FAT樣鈣黏蛋白等。它們的主要功能是介導細胞間Ca2+依賴的同型或異型黏附,而且涉及多種信號傳導包括Wnt/β-連環蛋白(β-catenin)、PI3K/Akt、Rho GTPase和NF-κB等通路,從而調控相互黏附細胞間的行為 [1-3]。
近年有許多研究表明,鈣黏蛋白的敲低或過表與多種疾病有關,如哮喘 [4]、慢性牙周炎 [5],動脈粥樣硬化 [6]、糖尿病 [7]等。在一些腫瘤的侵襲和轉移過程中,某些黏附分子介導的細胞黏附力降低在腫瘤細胞生物學行為中發揮著關鍵作用。例如,E-cadherin在多種腫瘤中被認為是抑癌基因,而N-Cadherin作為腫瘤侵襲的啟動子,被視為腫瘤細胞獲得侵襲性的必要條件 [8-10]。因此,鈣黏蛋白或可作為藥物靶點,成為治療過敏、自身免疫病及腫瘤的一種新的手段。
2. 什么是CDH17?
2.1 CDH17的結構
肝腸鈣黏蛋白(liver- intestine cadherin, Cadherin-17,又名CDH17;HPT-1;LI-Cadherin)是近年來新發現的一種鈣黏蛋白,其最早于1994年由Dietmar等通過分子克隆技術從鼠肝細胞cDNA文庫中分析得到的,由于在小鼠僅表達于肝臟和小腸,故命名為肝腸鈣黏蛋白 [11]。人CDH17基因定位于染色體8q22. 1,其結構與鈣黏蛋白家族成員具有同源性,但CDH17又有以下獨特的結構:①CDH17的胞外部分含有7個鈣黏蛋白重復區域,而經典鈣黏蛋白和橋粒鈣黏蛋白為5個;②在CDH17氨基末端的細胞黏附識別區內,決定細胞黏附特性的HAV序列由AAL序列代替;③CDH17細胞質尾僅含有20個氨基酸殘基,經典鈣黏蛋白有150-160個。因此,CDH17被劃分為經典鈣黏蛋白的變異體 (圖1) [12-14]。
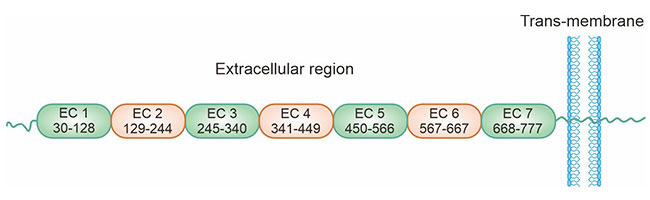
圖1. CDH17的結構 [14]
2.2 CDH17的表達及功能
CDH17主要表達于胚胎、成人腸上皮細胞和部分胰腺導管上皮細胞,在健康人群肝細胞、食管上皮細胞及胃黏膜中幾乎不表達 [15-18]。CDH17在細胞黏附過程中充當了與鈣黏蛋白同樣重要的角色,CDH17可直接與細胞支架連接,發揮其細胞黏附作用,而經典的鈣黏蛋白必須與鏈蛋白結合形成復合體才能發揮其黏附功能 [19-20]。在一些病理情況下,CDH17可表達于其它組織。目前研究發現,CDH17在胃癌、結直腸癌、肝癌、胰腺癌和膽管癌等多種腫瘤組織中均有不同程度的表達,CDH17的高水平表達與患者預后和風險評估密切相關 [21-23]。
3. CDH17在腫瘤中的作用機制
CDH17作為鈣黏蛋白超家族中的獨特一員,在多種疾病中均發現CDH17的異常表達。研究揭示CDH17的功能紊亂與腫瘤細胞的外周浸潤及轉移關系密切,對腫瘤的復發及患者的生存率均有影響。然而,目前對于CDH17與腫瘤相關作用機制尚未闡明。
在胃癌中,CDH17高表達可使E-cadherin/catenin復合物失去穩定而解離 [23]。研究已證實β-catenin和E-cadherin/catenin復合物通過Wnt信號傳導途徑參與胃癌的發生發展 [24-25]。此外,CDH17表達上調可影響GSK3的活性,抑制β-catenin-AXIN-APC-GSK3復合物的形成,穩定β-catenin表達水平,可使其與轉錄因子LEF/TCF結合,誘導Cyclin D1的產生,從而促進細胞增殖,抑制細胞凋亡(圖2) [26]。有研究認為β-半乳糖苷結合蛋白Galectin-3在胃癌侵襲過程中的異常表達對CDH17起調控作用,但具體調控機制有待進一步研究 [27-28]。
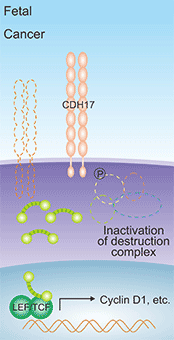
圖1. CDH17誘導Cyclin D1的產生 [26]
此外,利用慢病毒介導的microRNA干擾技術發現,抑制CDH17表達后,MMP-2和MMP-9的活性明顯降低,說明CDH17表達上調可增強MMP-2和MMP-9的活性,導致細胞外基質的降解和重塑,利于腫瘤細胞的轉移 [17]。另有報道,CDH17通過整合Ras/Raf/MEK/ERK信號通路,在胃癌細胞的增殖和腫瘤的生長中發揮重要作用(圖3) [29]。在肝癌中,敲低CDH17表達,導致Wnt/β-catenin信號通路失活,腫瘤生長受到抑制,因此推測靶向CDH17可滅活Wnt信號通路并激活抑癌基因,促進腫瘤細胞的凋亡 [30]。
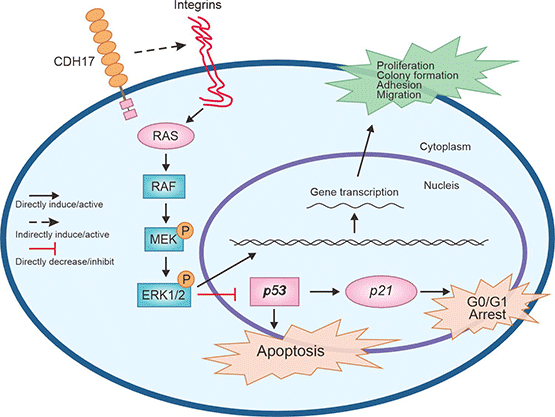
圖3. CDH17介導Ras/Raf/MEK/ERK信號通路 [29]
4. CDH17在癌癥治療中的作用
CDH17作為新型鈣黏蛋白,在細胞粘附、細胞識別、組織器官的發育和形態的維持等方面發揮重要作用。細胞間的粘附及運動能力的失調是腫瘤發生發展的重要機制之一。近年來有關于CDH17與腫瘤關系的靶向研究越來越多,主要見于胃癌、肝癌、結腸癌及胰腺癌等胃腸道惡性腫瘤。
4.1 CDH17和胃癌
CDH17最早被發現在胃癌中過度表達。臨床研究中,對71例胃癌患者的癌組織和正常胃組織進行半定量PCR、免疫組化及Western blot分析發現CDH17的表達水平與胃癌的組織學類型、腫瘤侵襲和淋巴結轉移均呈正相關。在CDH17過表達的BGC-823細胞株中,胃腺癌的增殖、侵襲及遷移能力增強。RNA干擾CDH17表達,發現下調CDH17能夠抑制MKN-45胃癌細胞的增殖、粘附和侵襲能力,同時NF-κB信號轉導通路被抑制、其下游蛋白(VEGF-C和MMP-9)減少 [31-33]。
4.2 CDH17和肝癌
研究表明CDH17與肝癌發生也有一定的關系。采用RT-PCR方法對57例肝癌組織及正常肝組織進行分析,結果顯示CDH17在肝癌組織中的陽性表達率顯著高于正常肝組織,說明CDH17與肝癌的發生有關,提示CDH17可能作為早期診斷肝癌的腫瘤標志物 [34]。對34例肝內膽管癌研究發現CDH17表達與腫瘤的分化程度和血管侵犯有關,敲除CDH17,發現CDH17表達下調,促進血管生成有關的MTF-1和胎盤生長因子PLGF的表達,進而誘導腫瘤血管生成 [11, 35]。另有研究發現CDH17的剪接異構體和基因多態性增加正常人群肝癌的發生風險 [26]。
4.3 CDH17和結腸癌
一項對45例結腸癌標本的研究發現,CDH17的表達下調與結腸癌的進展及淋巴結轉移有顯著關系。下調結腸癌細胞中CDH17基因的表達水平,可以抑制結腸癌細胞的侵襲和轉移過程。對原發部位的結腸癌組織和其轉移部位的癌組織中CDH17表達進行比較,發現二者之間的表達一致。因此,CDH17有望成為結腸癌轉移檢測的標志物 [22, 36]。
4.4 CDH17和食管癌
有研究分析食管癌組織中CDH17的表達情況與食管癌患者臨床特征的關系,發現在分化良好的食管癌組織中有較高的CDH17免疫反應,而低分化的食管腺癌組織中CDH17的表達水平較低或表達不明顯,證明食管腺癌的CDH17免疫反應與患者的臨床特征具有一定的關系 [37]。在食管鱗狀細胞癌ESCC中,CDH17 CpG 島甲基化狀態增強,CDH17表達水平降低,CDH17 CpG 島的甲基化狀態與CDH17的表達呈負相關 [38-39]。因此,CDH17可成為食管癌治療的新靶點。
4.5 CDH17和胰腺癌
一項對胰腺導管癌患者CDH17表達情況的研究發現,高分化癌中CDH17表達高于低分化癌者,Kaplan-Meier曲線分析表明CDH17高表達與患者預后生存有關 [40]。低CDH17表達與腫瘤去分化相關,由于相關研究甚少,因而CDH17與胰腺癌臨床病理特征及預后之間的關系還有待進一步探討。
4.6 CDH17和其它癌癥
對CDH17與卵巢上皮癌關系的研究發現,CDH17在低分化、高分期的腫瘤中高表達 [41]。單變量分析表明,CDH17高表達與預后不良有關。在導管內乳頭狀粘液性腫瘤(IPMN)中,CDH17誘導IPMN的腸型分化及癌變,隨著IPMN級別的增高,CDH17與之呈正相關 [42]。總而言之,陸續的研究提示CDH17可能成為胃癌、肝癌和結直腸癌等惡性腫瘤診斷和預后的標志物,監測腫瘤的進展及復發。
5. CDH17的臨床研究前景
目前已有多款基于CDH17的臨床藥物在研(表1),主要用于胃腸道腫瘤治療。其中,3款為雙特異性抗體:ARB-202(CDH17 x CD3),ARB-001.T(CDH17 x CD3),BI-905711(CDH17 x DR5/TRAIL-R2);1款CAR-T藥物CHM-2101;2款單抗。晚期消化道惡性腫瘤的治療,往往是以化療為基礎的單藥或聯合治療方案,雖然化療藥物及聯合治療策略迭代更新,但療效始終未能獲得突破性進展。腫瘤靶向免疫治療提供了全新高效、安全、低毒的治療策略,有望改變目前困境。現有研究成果已表明,靶向干擾CDH17可以抑制腫瘤生長。因此,CDH17作為新發現的肝腸鈣黏蛋白,正成為胃腸道腫瘤靶向治療的熱門靶點!
| 藥物 | 靶點 | 作用機制 | 藥物類型 | 在研適應癥 | 在研機構 | 最高研發狀態 |
|---|---|---|---|---|---|---|
| ARB-202 | CDH17;CD3 | 免疫調節劑; CDH17調節劑;CD3調節劑 |
雙特異性抗體 | 膽管癌; 結直腸癌; 胃腸道腫瘤;胃癌;膽道腫瘤;胰腺癌;肝癌;胰腺腺泡癌 |
Arbele | 臨床1期 |
| BI-905711 | DR5;CDH17 | DR5激動劑; CDH17調節劑 |
雙特異性抗體 | 彌漫性大B細胞淋巴瘤; 胃癌; 膽管癌;胃腸道腫瘤;胰腺癌;食管癌;膽管癌 |
C.H. Boehringer Sohn AG & Co. KG;勃林格殷格翰(中國)投資有限公司 Boehringer Ingelheim (China) Investment Co., Ltd.;勃林格殷格翰 Boehringer Ingelheim GmbH |
臨床1期 |
| Anti-CDH17 mAbs (ProAlt) | CDH17 | CDH17調節劑 | 單克隆抗體 | 轉移性結直腸癌;轉移性黑色素瘤 | 普羅克拉拉生物科學股份有限公司 Proclara Biosciences, Inc. |
臨床前 |
| ARB-001.M | CDH17 | CDH17拮抗劑 | 雙特異性抗體 | 胃腸道腫瘤 | Arbele | 臨床前 |
| ARB-001.T | CD3;CDH17 | CDH17調節劑 | 雙特異性抗體 | 結直腸癌;肝癌; 胃癌 |
Arbele | 臨床前 |
| ARB-201 | CDH17 | CDH17拮抗劑;CD3抑制劑 | 雙特異性抗體 | 結直腸癌 | Arbele | 臨床前 |
| CHM-2101 | CDH17 | CDH17調節劑;基因轉移 | CAR-T | 結直腸癌; 胃腸道腫瘤; 神經內分泌腫瘤 |
/ | 臨床前 |
| CHM-2301 | CDH17 | CDH17調節劑 | CAR-NK | 實體瘤 | / | 臨床前 |
| Anti-CDH17-based antibody drug conjugates(ProAlt) | CDH17 | CDH17調節劑 | ADC;單克隆抗體 | 結直腸癌 | Protein Alternatives SL | 藥物發現 |
表1:CDH17的臨床藥物在研
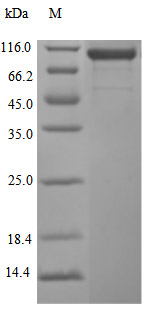
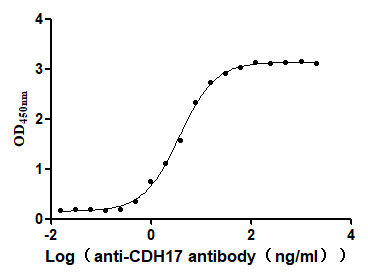
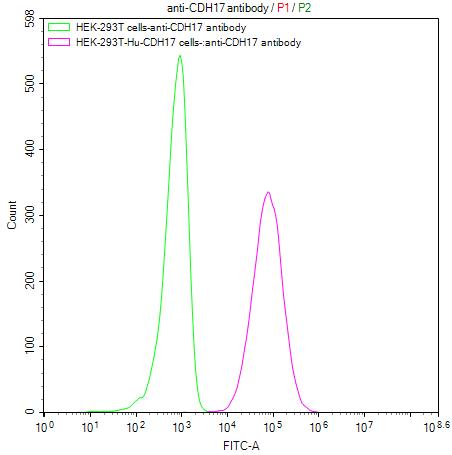
為鼎力協助各藥企針對CDH17在胃腸道腫瘤等其它腫瘤在臨床中的研究,CUSABIO推出CDH17活性蛋白產品,(Code:CSB-MP613267HU),助力您在CDH17機制方面的研究或其潛在臨床價值的探索。
CDH17 Protein&Human CDH17 Stable Cell Line
參考文獻:
[1] Hulpiau, Paco, Ismail Sahin Gul, and Frans Van Roy. "Evolution of cadherins and associated catenins. "The Cadherin Superfamily: Key Regulators of Animal Development and Physiology (2016): 13-37.
[2] Ma, Yi-Shih, et al. "Bisdemethoxycurcumin suppresses human osteosarcoma U-2 OS cell migration and invasion via affecting the PI3K/Akt/ NF-κB, PI3K/Akt/GSK3β and MAPK signaling pathways in vitro." Oncology Reports 48.6 (2022): 1-10.
[3] Yu, Weina, et al. "Cadherin signaling in cancer: its functions and role as a therapeutic target." Frontiers in oncology 9 (2019): 989.
[4] Türkeli, Ahmet, et al. "Anti-VEGF treatment suppresses remodeling factors and restores epithelial barrier function through the E -cadherin/β-catenin signaling axis in experimental asthma models." Experimental and Therapeutic Medicine 22.1 (2021): 1 -9.
[5] Ramesh, P. K. Immunolocalization of Gingival E-Cadherin Expression in Smokers and Non-Smokers with Chronic Periodontitis. diss. KSR Institute of Dental Science and Research, Tiruchengode, 2020.
[6] Harki, Olfa, et al. "Inhibition of Vascular Endothelial Cadherin Cleavage Prevents Elastic Fiber Alterations and Atherosclerosis Induced by Intermittent Hypoxia in the Mouse Aorta." International Journal of Molecular Sciences 23.13 (2022): 7012.
[7] Koziolek, Michael, et al. "Urine E-cadherin: a marker for early detection of kidney injury in diabetic patients." journal of clinical medicine 9.3 (2020 ): 639.
[8] Loh, Chin-Yap, et al. "The E-cadherin and N-cadherin switch in epithelial-to-mesenchymal transition: signaling, therapeutic implications, and challenges." Cells 8.10 (2019): 1118.
[9] Yu, Chong, et al. "The lncRNA ZNF667-AS1 Inhibits Propagation, Invasion, and Angiogenesis of Gastric Cancer by Silencing the Expression of N-Cadherin and VEGFA." Journal of Oncology 2022 (2022).
[10] Zhang, Jinyao, et al. "Clinical significance of ALDH1A1 expression and its association with E-cadherin and N-cadherin in resected large cell neuroendocrine carcinoma." Translational Oncology 19 (2022): 101379.
[11] Takamura, Masaaki, et al. "Involvement of liver-intestine cadherin in cancer progression." medical molecular morphology 46 (2013): 1-7.
[12] Ordóñez, Nelson G. "Cadherin 17 is a novel diagnostic marker for adenocarcinomas of the digestive system." Advances in anatomic pathology 21.2 (2014): 131-137.
[13] Gray, Michelle E., and Marcos Sotomayor. "Crystal structure of the nonclassical cadherin-17 N-terminus and implications for its adhesive binding mechanism." Acta Crystallographica Section F: Structural Biology Communications 77.3 (2021): 85-94.
[14] Caporuscio, Christian, et al. "Immunoaffinity enrichment LC-MS/MS quantitation of CDH17 in tissues." Bioanalysis 12.20 (2020): 1439- 1447.
[15] Horsfield, Julia, et al. "Cadherin-17 is required to maintain pronephric duct integrity during zebrafish development." Mechanisms of development 115.1-2 (2002): 15-26.
[16] Huang, Li-Ping, et al. "Up-regulation of cadherin 17 and down-regulation of homeodomain protein CDX2 correlate with tumor progression and unfavorable prognosis in epithelial ovarian cancer." International Journal of Gynecologic Cancer 22.7 (2012).
[17] Jiang, Xiao-jie, et al. "CDH17 alters MMP-2 expression via canonical NF-κB signalling in human gastric cancer." Gene 682 (2019): 92-100.
[18] Liu, Xinjian, et al. "Disruption of oncogenic liver-intestine cadherin (CDH17) drives apoptotic pancreatic cancer death." Cancer Letters 454 (2019): 204-214.
[19] Xia, Peng, et al. "Surface-Engineered Extracellular Vesicles with CDH17 Nanobodies to Efficiently Deliver Imaging Probes and Chemo -Photothermal Drugs for Gastric Cancer Theragnostic." Advanced Functional Materials (2022): 2209393.
[20] Xia, Peng, et al. "Surface-Engineered Extracellular Vesicles with CDH17 Nanobodies to Efficiently Deliver Imaging Probes and Chemo -Photothermal Drugs for Gastric Cancer Theragnostic." Advanced Functional Materials (2022): 2209393.
[21] Feng, Zijie, et al. "Potent suppression of neuroendocrine tumors and gastrointestinal cancers by CDH17CAR T cells without toxicity to normal tissues." Nature Cancer 3.5 (2022): 581-594.
[22] Pei, Xiao Meng, et al. "The diagnostic significance of CDH17-positive circulating tumor cells in patients with colorectal cancer." Expert Review of Molecular Diagnostics just-accepted (2023).
[23] Wu, Cunen, et al. "Interaction between Wnt/β-catenin pathway and microRNAs regulates epithelial-mesenchymal transition in gastric cancer." International journal of oncology 48.6 (2016): 2236-
[22] 6.
[24] Kaszak, Ilona, et al. "Role of cadherins in cancer-a review." international journal of molecular sciences 21.20 (2020): 7624.
[25] Wang, Qianwen, et al. "MICAL2 contributes to gastric cancer cell migration via Cdc42-dependent activation of E-cadherin/β-catenin signaling pathway ." Cell Communication and Signaling 20.1 (2022): 136.
[26] Lee, Nikki P., et al. "Role of cadherin-17 in oncogenesis and potential therapeutic implications in hepatocellular carcinoma. "Biochimica et Biophysica Acta (BBA)-Reviews on Cancer 1806.2 (2010): 138-145.
[27] Huang, Hsiang-Wei, et al. "Association between inflammation and function of cell adhesion molecules influence on gastrointestinal cancer development." Cells 10.1 (2021): 67.
[28] Maher, John, and David M. Davies. "CAR-Based Immunotherapy of Solid Tumours-A Survey of the Emerging Targets. "Cancers 15.4 (2023): 1171.
[29] Lin, Zhaohu, et al. "Targeting cadherin-17 inactivates Ras/Raf/MEK/ERK signaling and inhibits cell proliferation in gastric cancer." PLoS One 9.1 ( 2014): e85296.
[30] Wang, Yonggang, et al. "Anti-cadherin-17 antibody modulates beta-catenin signaling and tumorigenicity of hepatocellular carcinoma." ploS one 8.9 ( 2013): e72386.
[31] Motoshita, Junichi, et al. "Molecular characteristics of differentiated-type gastric carcinoma with distinct mucin phenotype: LI -cadherin is associated with intestinal phenotype." Pathology international 56.4 (2006): 200-205.
[32] Wang, Jin, et al. "Cadherin-17 induces tumorigenesis and lymphatic metastasis in gastric cancer through activation of NFκB signaling pathway." Cancer biology & therapy 14.3 (2013): 262-270.
[33] Qiu, Hai-bo, et al. "Targeting CDH17 suppresses tumor progression in gastric cancer by downregulating Wnt/β-catenin signaling." ploS one 8.3 (2013): e56959.
[34] Su, Min-Cheng, et al. "Cadherin-17 is a useful diagnostic marker for adenocarcinomas of the digestive system." Modern Pathology 21.11 (2008): 1379- 1386.
[35] Takamura, Masaaki, et al. "Loss of liver-intestine cadherin in human intrahepatic cholangiocarcinoma promotes angiogenesis by up-regulating metal- responsive transcription factor-1 and placental growth factor." International journal of oncology 36.1 (2010): 245-254.
[36] Harding, J. J., et al. "371P A phase Ia/b, open-label, multicentre study of the TRAILR2 agonist BI 905711 in patients (pts) with advanced gastrointestinal (GI) cancers." Annals of Oncology 33 (2022): S706.
[37] Panarelli, Nicole C., et al. "Tissue-specific cadherin CDH17 is a useful marker of gastrointestinal adenocarcinomas with higher sensitivity than CDX2 ." American journal of clinical pathology 138.2 (2012): 211-222.
[38] Shenoy, U. Sangeetha, et al. "Molecular implications of HOX genes targeting multiple signaling pathways in cancer." Cell biology and toxicology (2022) : 1-30. : 1-30.
[39] Ignatova, Ekaterina Olegovna, et al. "Clinical significance of molecular subtypes of gastrointestinal tract adenocarcinoma." World Journal of Gastrointestinal Oncology 14.3 (2022): 628.
[40] Liu, Xinjian, et al. "Disruption of oncogenic liver-intestine cadherin (CDH17) drives apoptotic pancreatic cancer death." Cancer Letters 454 (2019): 204-214.
[41] Huang, Li-Ping, et al. "Up-regulation of cadherin 17 and down-regulation of homeodomain protein CDX2 correlate with tumor progression and unfavorable prognosis in epithelial ovarian cancer." International Journal of Gynecologic Cancer 22.7 (2012).
[42] Karimi, S. S., T. Valyi-Nagy, and M. F. Gonzalez. "TTF-1 Immunoexpression in Primary Rectal Adenocarcinoma with Brain Metastasis. "American Journal of Clinical Pathology 156.Supplement_1 (2021): S63-S63.